Overview
With an influx of funding for public health infrastructure becoming available, states have the opportunity to implement the Foundational Public Health Services (FPHS) across their public health systems. A key component to accomplish this implementation is assessing the current capacity and cost to deliver capabilities and programs that no jurisdiction can be without. This assessment estimates the gap between current investments and capacity, which states can use to determine what would be needed for full implementation systemwide.
Process
There are several important steps states should consider when preparing to assess the current capacity and cost of their systems.
- Identify and engage all parts of the governmental public health system. Each state defines its governmental public health system differently, which could include the state health agency, local health departments, Tribal nations (in collaboration with and with consideration around Tribal sovereignty), governing entities, and others who have the authority to provide public health services statewide. This step allows states to understand who they are conducting the assessment and costing process with and how to interpret results specific to their state context.
- Identify the resources necessary to conduct the assessment. Resources needed to complete the assessment could consist of engaging a contractor or partner to develop and implement the assessment or deciding to do this work with in-house staff time. This step allows states to determine if they can currently implement this task or need to obtain the resources to do so.
- Establish methods to conduct the assessment. In reviewing the national FPHS definitions, states will need to determine if adopting them or modifying them for a state-specific version meets their goals. In addition, states will need to develop planning criteria to help guide the process, like designing/tailoring the assessment tool, developing and implementing the assessment activities, providing training and technical assistance, reviewing and analyzing the results, and preparing reports and other materials. This step allows states to map capabilities and areas to their definitions, and ultimately how they can match results to the costing piece of the process.
- Complete the staffing capacity and financial assessment tool to determine the level of FPHS implementation and the current investments by capability and program. Detailing the current levels of capabilities and programs within the system is important for states to understand the baseline of FPHS implementation systemwide. This step allows states to collect actual data and analyze it, then approximate what is needed to fill any gaps identified.
- Estimate the staffing and funding needed for full implementation and develop recommendations for funding. Based on the results of the assessment, states will have a better understanding of gaps and what is needed to support the FPHS. This step allows states to use the assessment data to initiate statutory changes and develop legislative asks.
Examples
Several states that are part of the 21st Century (21C) Learning Community have undertaken an assessment process that has resulted in real impact, with a few examples below.
Washington
In 2016, Washington conducted an assessment to understand current statewide implementation and spending on FPHS and to estimate the cost to fully provide FPHS statewide. This assessment was the first attempt to collect data from the Washington State Department of the Health, the Washington State Board of Health, and all 35 local health jurisdictions to inform public health leaders in designing and implementing a transformed public health system to better serve the people in the state. The assessment was designed to cover all activities within the FPHS framework and resulted in a long and detailed data collection tool, which agencies found challenging to complete given their current workload and capacity.
The assessment revealed that no foundational program or capability is fully or significantly implemented across all responding agencies, suggesting that FPHS in Washington do not currently meet the condition of “must exist everywhere, to work anywhere.” There are gaps across the system in all agencies of all sizes, which are not uniform, nor do they appear in the same places in every organization.

Washington State Public Health Transformation Assessment Report for State and Local Public Agencies, September 2018. https://wsalpho.box.com/s/j5d2xon6w25oj31q0gwr1qy6xqn2io4o
The assessment determined the cost of full FPHS implementation in Washington is $595 million, and the system was currently spending $368 million. Thus, the additional funds needed to fill the gap is approximately $227 million annually.
Oregon
Also in 2016, Oregon conducted an assessment to understand the state’s current capacity for providing foundational programs and capabilities and to estimate the cost to fully implement those foundational programs and capabilities. This assessment collected data from the Oregon Health Authority Public Health Division and all 34 local public health authorities to provide an overall indicator of the size, location, and nature of the programmatic gaps that currently exist in providing foundational programs and capabilities in all communities across the state.
The assessment revealed that no foundational program or capability is significantly implemented across all authorities, and there are gaps across the system in all authorities of all sizes.

State of Oregon Public Health Modernization Assessment Report, June 2016. https://www.oregon.gov/oha/PH/ABOUT/TASKFORCE/Documents/PHModernizationReportwithAppendices.pdf
The assessment determined the cost of full FPHS implementation in Oregon is $314 million, and the system was currently spending $209 million. Thus, the additional funds needed to fill the gap is approximately $105 million annually.
Ohio
Starting in 2017, Ohio took a different approach and determined that actual cost data, rather than cost estimates, would be more useful in their FPHS efforts. Local health departments in the state are required to submit Annual Financial Reports (AFRs), which presented the perfect opportunity to align cost categories with FPHS definitions to seamlessly provide data from all local health departments by FPHS category in a complete, standardized dataset. Pilot testing of this new AFR took place in 2018 and actual costs have analysis starting in 2019.
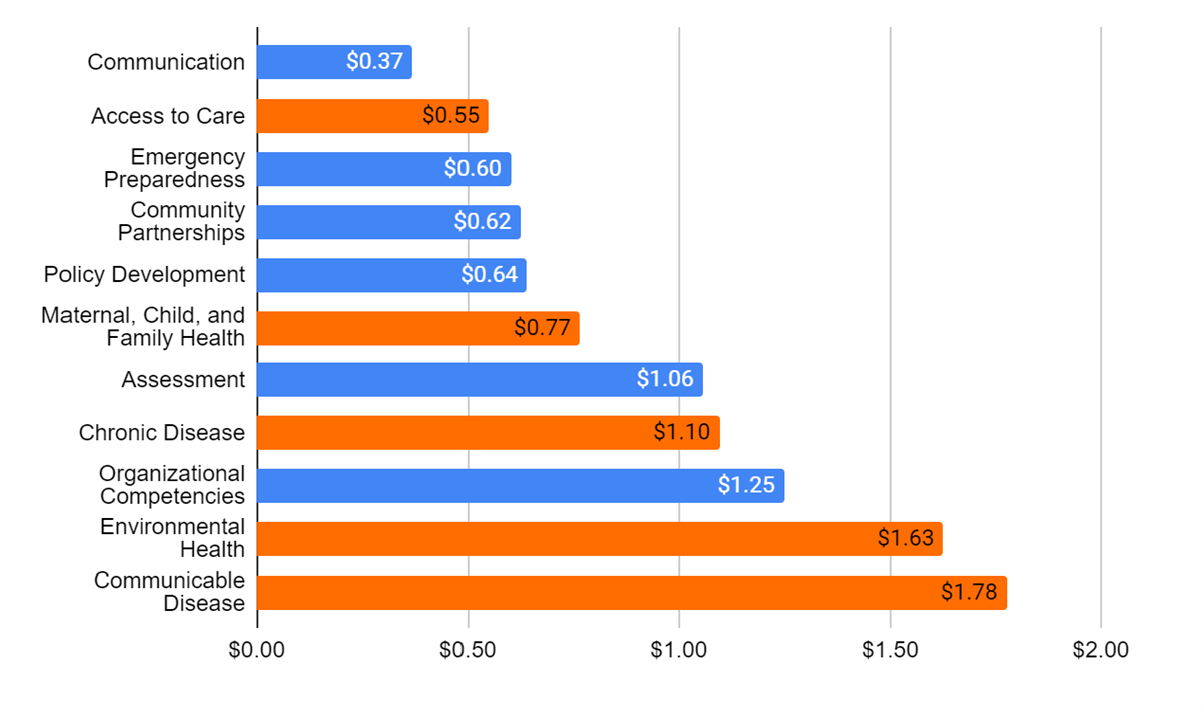
In FY 2019, Ohio health departments spent an average of $26.89 per capita on the FPHS: $11.76 per capita was spent on the Foundational Capabilities and $15.13 per capita was spent on the Foundational Areas. Based on these findings, an estimated annual investment of $10.35 per capita is needed to close existing funding gaps and fully implement the FPHS in Ohio: $4.54 per capita for implementing the Foundational Capabilities and $5.81 per capita for implementing the Foundational Areas.
Costing the FPHS in Ohio Analysis for FY 2019 Final Report, September 2021. https://www.ohiopublichealth.org/_files/ugd/7ddbf5_f7bcc1c3b6a446f2bdfda6c051c78b99.pdf
Based on the Ohio population of 11,690,000 residents in 2019, this translates into an annual investment need of approximately $121 million for all local health departments in the state ($53 million is needed to implement the Foundational Capabilities and $68 million is needed to implement the Foundational Areas).
Coming Soon
PHAB’s Center for Innovation is currently developing a capacity and cost assessment tool that state-wide health department systems can use to determine their level of current implementation of Foundational Capabilities and Foundational Areas and their associated costs. The assessment tool identifies the needed expertise and capacity to fully achieve improved organizational systems and processes to deliver the FPHS. More details on the FPHS Capacity and Costing Assessment Tool will be shared in the coming months.
AUTHOR: TRAVIS PARKER LEE, SENIOR SPECIALIST





